

The Brain Tumor Institute at Children’s National Hospital is home to internationally recognized experts dedicated to providing your child with a better quality of life after a brain tumor diagnosis.
Brain tumors are abnormal growths that disrupt the normal functioning of your child's brain and nervous system. These tumors are especially challenging in children because their brains are still developing, putting them at risk for lifelong complications. That’s why our approach goes beyond treating the tumor—we focus on preserving your child’s cognitive, emotional and physical development throughout their care journey.
To achieve this, our program brings together a uniquely integrated team of specialists who work side by side from diagnosis through recovery. This close collaboration allows us to create highly personalized treatment plans that reflect the latest advances in pediatric brain tumor care, while also supporting your child’s overall well-being.
Our Providers
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs.
Contact Information
For appointments, please call 1-888-884-BEAR (2327) and for information, call 202-476-3643. For urgent assistance outside of business hours, call 202-476-5000.
A World Leader in Childhood Brain Tumor Care and Research
The Brain Tumor Institute is pioneering novel therapies developed at Children's National, including new molecularly-targeted therapies, vaccines, T-cell immunotherapies and minimally invasive techniques. Our commitment to research provides your child with access to the latest, most effective treatments for brain tumors, saving lives and improving outcomes. In addition, we include your family in all treatment decisions.
Learn more about what sets us apart:
Who are the pediatric brain tumor specialists supporting your child’s journey?
What makes our pediatric brain tumor treatments among the most advanced in the nation?
What brain tumor clinical trials are available at Children's National?
How is Children's National using focused ultrasound as a minimally-invasive surgical treatment?
How do cognitive and emotional health play a role in brain tumor care?

Neuro-Oncology Clinic
The Brain Tumor Institute hosts weekly multidisciplinary neuro-oncology clinics for patients and families in Washington, D.C., and in Fairfax, Va.
This clinic includes providers from Oncology, Neurology, Endocrinology, Physical Medicine and Rehabilitation Medicine, Psychiatry and Clinical Nutrition Services. The ability to access all of these services in one convenient clinic exemplifies our efforts to streamline complex care for our patients. Established patients can call 202-476-3643 to schedule an appointment.


Understanding and Treating Pediatric Brain Tumors

What are brain tumors?
Brain tumors are abnormal growths of tissue in the brain, which may be benign (non-cancerous) or malignant (cancerous).

Getting a diagnosis
An accurate diagnosis is the foundation for any successful cancer treatment. At Children’s National, we ensure a precision diagnosis for every child.


Brain tumor treatments
Children's National offers the full range of pediatric brain tumor therapies, including surgery, radiation, chemotherapy and targeted therapies.

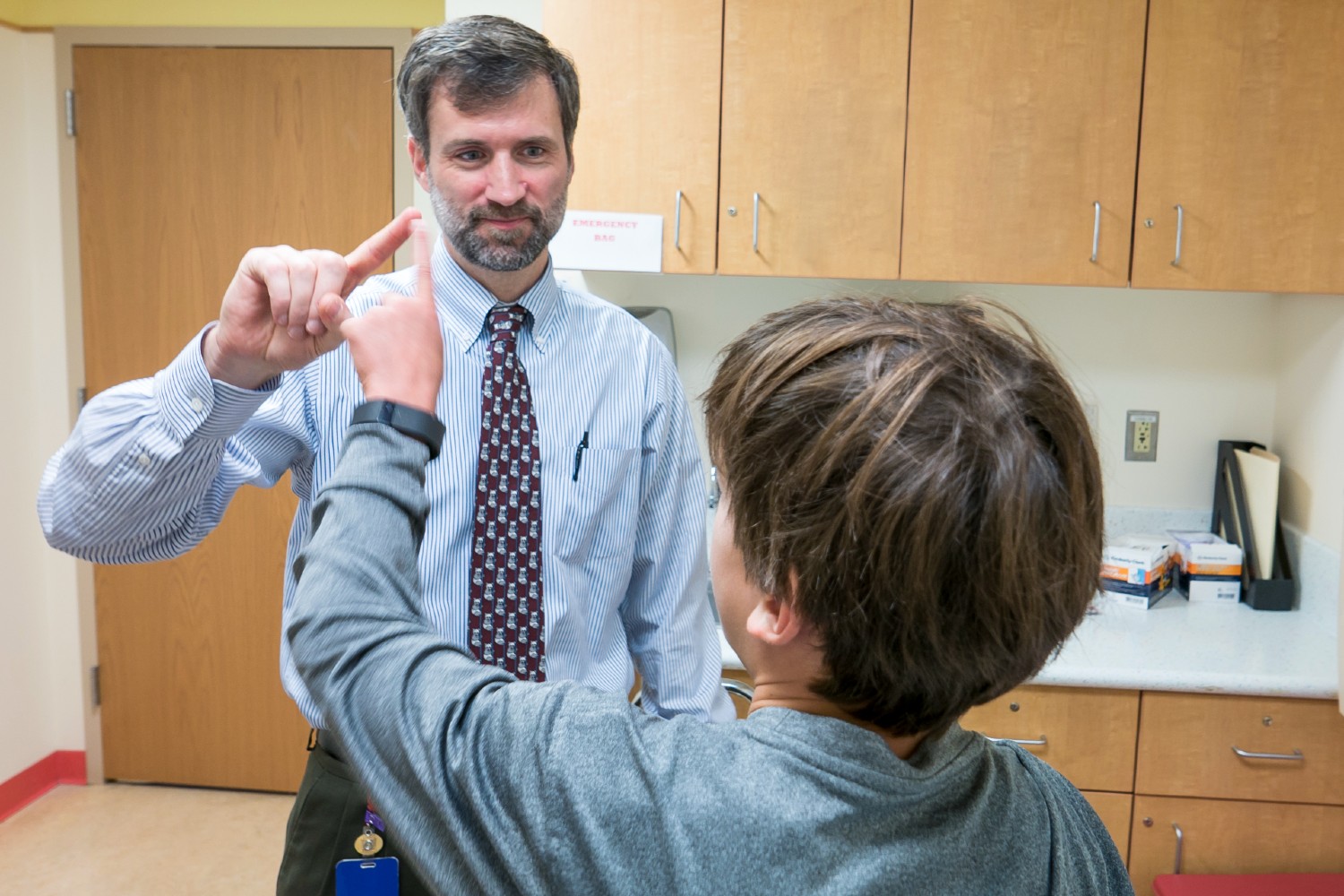
Our Team Approach to Pediatric Brain Tumors
To provide your child with the best possible care, we have assembled a team of pediatric experts. Together, these specialists meet regularly to create personalized treatment plans and provide advanced care to children with brain tumors. During a single clinic visit your child meets with a broad range of specialists from various departments, including:
From Brain Tumor Research to Patient Care
Learn more about the Brain Tumor Institute and its approach to treatment in this Q&A with Brian Rood, MD.
Pediatric Brain Tumor Research at Children’s National
Our researchers are pushing the scientific boundaries of pediatric brain tumor care, providing the latest, most promising diagnosis and treatment options to our patients.
Our Research
![]()
Our research has been recognized around the world and focuses on:
- Medulloblastoma, and other infantile embryonal tumors
- High-grade gliomas
- Low-grade gliomas, including chiasmatic, low grade, and optic nerve
- Ependymoma
- Atypical teratoid/ rhabdoid tumor
- Craniopharyngioma
- Germ cell tumors, including mixed germ cell tumors
- Late effects of brain tumors and their treatment
- Sellar tumors through our Pituitary and Skull Base Disorder Program
Our World-Class Network
![]()
Children’s National’s brain tumor clinical research is worldwide and we proudly serve as members of the world’s largest and most prestigious clinical trials networks, including:
- Childhood Brain Tumor Tissue Network
- Children's Oncology Group's Phase 1 Consortium
- Collaborative Ependymoma Research Network
- CONNECT Consortium
- Neurofibromatosis Clinical Trials Consortium (Department of Defense)
- Pacific/Pediatric Neuro-Oncology Consortium
- Pediatric Brain Tumor Consortium
- Remission (Immunotherapy) Consortium
Our Clinical Trials
![]()
At the Brain Tumor Institute at Children’s National, we’re not just treating brain tumors—we’re transforming the future of pediatric care. Through groundbreaking clinical trials, we offer families hope and access to innovative therapies that could make a life-changing difference for their child—and for countless others.
Locations
This is a carousel. Use Next and Previous buttons to navigate.

in the news
Former patient returns to Children’s National for powerful performance
Lydia Sutton was treated for a brain tumor as a teenager. Now, a student of music, she was invited back to the hospital to deliver a memorable show. (Story by WUSA9)














