Stakeholders recommend updates to newborn screening guidelines for critical congenital heart disease
Updates to screening protocol will refine algorithm and improve reporting for the standard newborn assessment
WASHINGTON – A distinguished panel of medical experts, state and federal health officials, and congenital heart disease parent advocates published recommended updates to the current American Academy of Pediatrics’ protocol for detecting critical congenital heart disease (CCHD) in newborn babies using pulse oximetry. The recommendations appear in the June 2020 issue of Pediatrics. Updates include:
- Key algorithm changes to simplify the passing threshold and trigger clinical assessment faster when a child’s oxygen saturation is low
- A call for an investment in public health infrastructure to allow for improved data collection of population level screening outcomes across states
- Increased education about the tool’s strengths and limitations
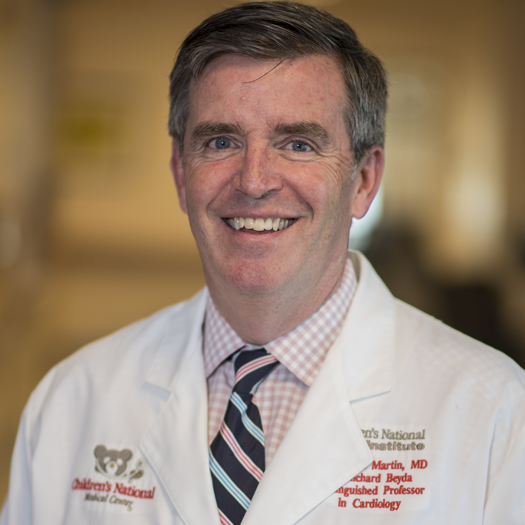
“In less than ten years, this non-invasive, low-cost screening tool and algorithm that started as a regional pilot program has become a critical part of the Recommended Uniform Screening Panel (RUSP) for every newborn in the United States,” says Gerard Martin, M.D., cardiologist at Children’s National Hospital and a lead author of the study recommendations. “We estimate that at least 120 babies’ lives are saved by this tool in the U.S. every year, and we think the tool can save even more as it grows to become a standard of newborn care around the world.”
Key algorithm changes
- Screening failed if oxygen saturation in hand OR foot is less than 95%. The panel found evidence to recommend a screening fail or retest if either the right hand or lower extremity shows an oxygen saturation of less than 95%. The current American Academy of Pediatrics (AAP) algorithm recommends both hand and foot saturations must be less than 95% or a difference of 3% between the two to trigger a retest or a screening fail.
- Eliminate second retest. Clinical assessment is now recommended after a newborn’s oxygen saturation does not meet passing criteria in the initial test and one retest. The current AAP algorithm calls for up to two retests to minimize false positives. However, the evidence showed that eliminating the second retest requirement ensures children who may need urgent attention are able to get assessed and treated sooner with fewer retests.
- Continue screening between 24 to 48 hours after birth. The panel decided the current recommended screening window between 24 and 48 hours after birth would remain the same given the increase in false positives when screening is completed too early. However, the recommendation acknowledges that completing screening before 24 hours has passed is acceptable in cases where early discharge of mother and baby is under consideration.
The panel considered several additional updates to the U.S. algorithm, but did not feel the evidence was strong enough to warrant further changes at this time.
Uniform public health CCHD reporting and clinician training
Though screening is required in all 50 states, the panel found that data collection is inconsistent across states. This makes it difficult to assess trends in effectiveness and identify any screening gaps on a national scale.
“Every state has done a good job of making sure that newborns are screened in the appropriate window,” says Matt Oster, M.D., MPH, director of the Cardiac Outcomes Research Program at Children’s Healthcare of Atlanta, and another study author. “However, variations in reporting, including in the definition of critical congenital heart disease make it difficult to know precisely how effective the tool is. It’s critical that we help public health programs focus on protocol adherence and standardize data collection so we can accurately gauge the cases we capture and those we miss.”
Training for providers; education for parents
The panel also emphasized the importance of making sure every care provider is trained to administer and record results in a uniform way.
As part of the RUSP in the United States, every baby born is required to receive the pulse oximetry screening within the first 24 to 48 hours, along with a battery of other screening tools.
“We need to do a better job of explaining to parents that a failed pulse oximetry screen simply triggers a closer clinical assessment,” Dr. Martin says. “It doesn’t indicate a specific issue other than a low level of oxygen saturation in the infant’s body. Further clinical evaluation will tell us more and help us find any diagnosis.”
The future of pulse oximetry to detect CCHD
Pulse oximetry screening continues to grow in the United States and other countries. The panel recommended a continuing effort by organizations such as the AAP, the American College of Cardiology and the American Heart Association to lead implementation of this inexpensive screening tool around the world. In 2014, the World Health Organization estimated that doing so might save more than 750,000 lives by the year 2030.
Media Contact
Related Departments
This is a carousel. Use Next and Previous buttons to navigate, or jump to a slide with the slide dots.