Research
Fellows are exposed to faculty research activities early in their first year and then meet with program leadership to discuss their research interests and facilitate meetings with potential mentors based on shared interests. Mentors draw from both the Division of Neonatology and the broader Children’s National Research Institute. Once successfully paired with a faculty research mentor, fellows will meet regularly with their mentor and are assigned a Scholarship Oversight Committee (SOC) consisting of faculty members with interests and expertise in either clinical, epidemiological and health services research, or basic science and translational research, according to the fellow’s scholarly objectives.
Fellows present their scholarly progress to their SOC semiannually (or more frequently as needed) and receive constructive feedback, support and encouragement to ensure the requirements of the American Board of Pediatrics have been met.
Explore Faculty Research Interests
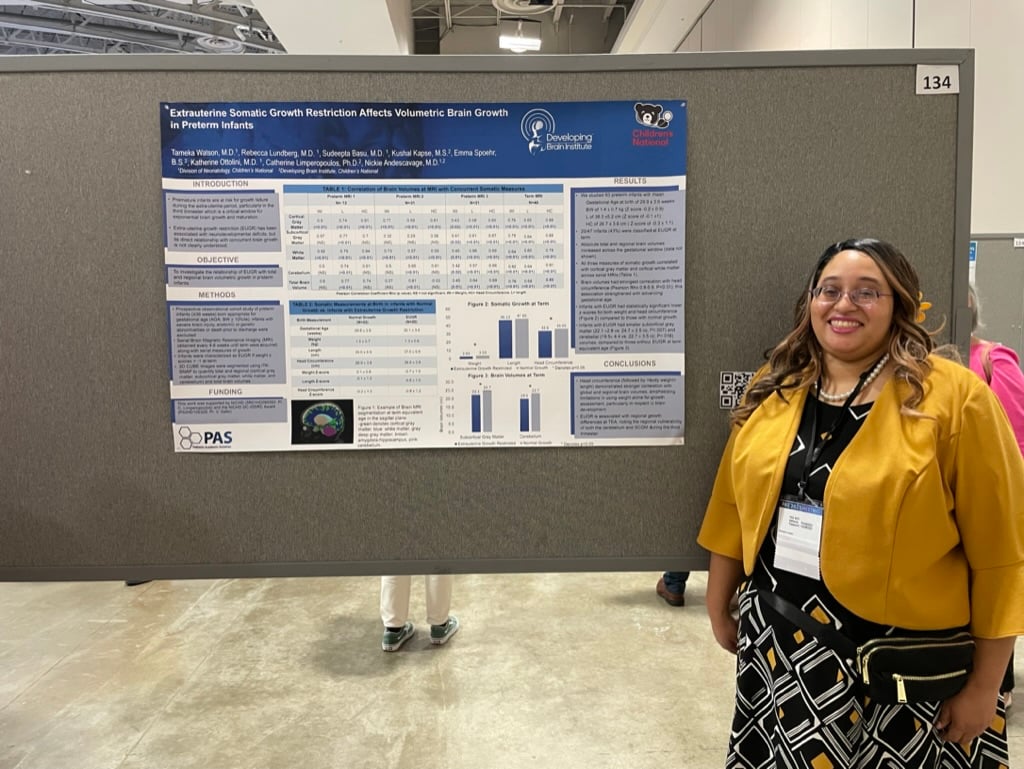
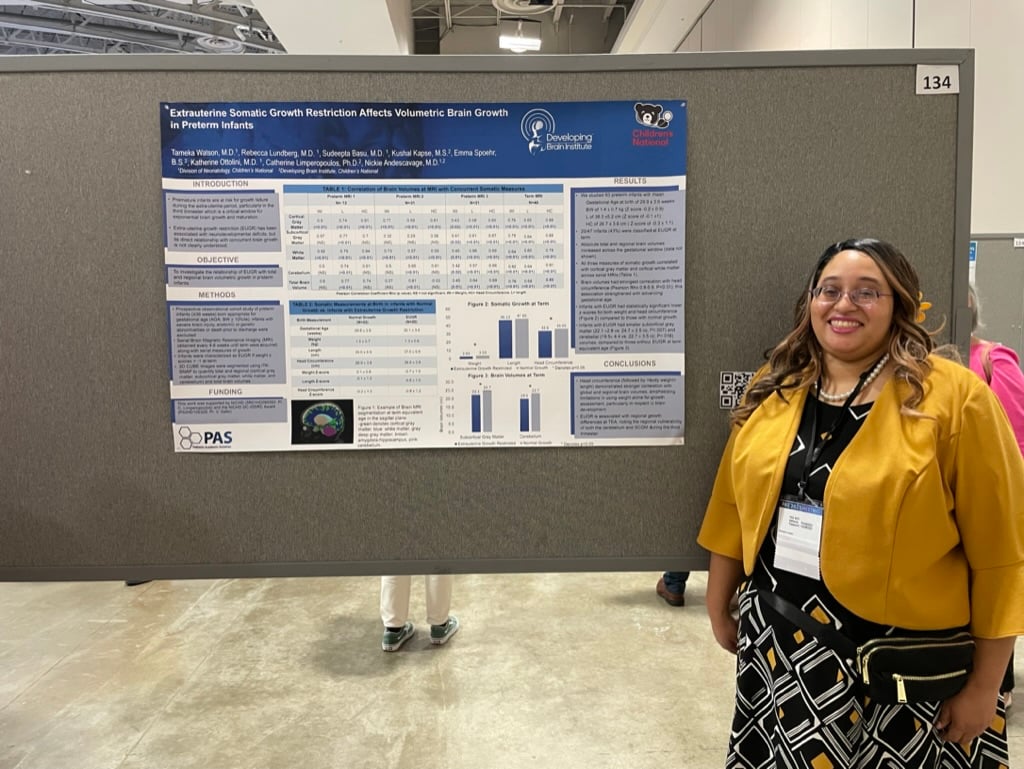
Nickie Niforatos Andescavage, MD
Associated Facility: Children's National Hospital
Dr. Andescavage completed fellowships in Neonatal-Perinatal Medicine as well as Fetal-Transitional Medicine. She serves as the associate chief of the Developing Brain Institute and director of the Maternal-Infant Clinical Trials Unit. Her research areas of interest include intrauterine development in healthy and high-risk pregnancies, specifically placental health and fetal-neonatal neurodevelopment, as well as the role of maternal exposures on feto-placental health.
Elisabeth A. Anson, MD
Associated Facility: Children's National Hospital
Dr. Anson completed residency training, a chief residency and Neonatal-Perinatal fellowship at Children’s National Hospital. She is the medical director for the Neonatal Transport Team, focusing on community outreach neonatal education and advocacy for newborns at both the local District of Columbia and national levels. She greatly enjoys educating and mentoring residents and fellows and is passionate about trainee wellness. She also has a specific interest in neonatal palliative care.
Sudeepta Kumar Basu, MD
Associated Facility: Children's National Hospital
Dr. Basu is an associate professor of pediatrics at The George Washington University School of Medicine and Health Sciences. His research focus relates to understanding brain injury and development in preterm infants using advanced monitoring tools including magnetic resonance imaging (MRI) and video encephalography. In collaboration with the Developing Brain Institute, he has adapted advanced MRI techniques to measure in vivo concentrations of GABA in preterm brain. One of the key areas of research is monitoring sleep-cycle maturation in preterm infants and how the NICU environment impacts it during their NICU stay and early infancy. Understanding the interaction between postnatal exposures in the NICU with concurrent brain development is the key to elucidating early biomarkers of brain injury. His previous investigations include the role of glycemic homeostasis in infants with perinatal asphyxia and its influence on brain injury and outcomes.
Sweta Bhargava, MD, FAAP
Associated Facility: Children's National Hospital
Dr. Bhargava is an assistant professor of pediatrics at The George Washington University School of Medicine and Health Sciences. Her research interest is in neonatal hemodynamics and in the use of point-of-care ultrasound (POCUS) in the NICU. In her previous post at NYU, she demonstrated the feasibility of creating a POCUS training curriculum for neonatal providers and continues with this initiative at the current institute. She has experience in using simulation, technology and quality improvement methodologies to improve procedural skills in the NICU. She is a part of working group addressing neonatal PICC practices and policies. She remains actively involved in resident and fellow education. She is a member of the American Academy of Pediatrics and the American Society of Echocardiography. She is a part of our nocturnal neonatal attending team.
Natalia Andrea Isaza Brando, MD
Associated Facility: Children's National Hospital & George Washington Hospital
Dr. Isaza’s interests have focused on the study of the effect of skin-to-skin contact, and the benefit this provides the NICU patients and their parents. She is a member of the neonatology nocturnal care team, providing oversite of the resident and fellows on the night shift. She is also the neonatal lead for the neurodevelopmental follow-up clinic. She has championed family support and education on discharge to home planning for our families and provided classes in Spanish for our Spanish speaking families.
Kelsey Elizabeth Donoho, MD
Associated Facility: Children's National Hospital
Dr. Donoho is an assistant professor of pediatrics at The George Washington University School of Medicine and Health Sciences. She earned her medical degree from the University of California, Irvine, and completed her residency training at Children’s Hospital Los Angeles and her Neonatal-Perinatal fellowship from Los Angeles County University of Southern California Medical Center. She is the director of point-of-care-ultrasound (POCUS) in the NICU at Children’s National, overseeing fellow education in POCUS as well as supervision for its use in the clinical and research domains. Her clinical research interest focuses on the use of assistive technology to improve procedural use of POCUS in the NICU. She is also the director of the PICC Team in the NICU. She also has an interest in quality improvement and is conducting multiple quality improvement studies in the NICU.
Mojgan Ghazirad, MD
Associated Facility: George Washington Hospital
Dr. Ghazirad graduated from Tehran University of Medical Sciences in 2000. She studied pediatrics at Inova Children’s Hospital and received her neonatal-perinatal medicine subspecialty from George Washington University in 2013. She currently works as an assistant professor of pediatrics at George Washington University NICU in Washington, D.C. She is interested in delivery room management of the critically ill premature or term newborn and has been teaching the skill to pediatric residents for many years. Currently she is working on quality improvement projects such as developing an effective algorithm for diagnosing and preventing early onset sepsis in newborns.
Suma Bhat Hoffman, MD, MS
Associated Facility: Children's National Hospital
Dr. Hoffman is the associate program director of the Neonatal-Perinatal Fellowship Program and associate professor of pediatrics at The George Washington University School of Medicine and Health Sciences. She completed both pediatric residency and Neonatal-Perinatal fellowship training at Children’s National Hospital and then went on to serve as faculty in the Department of Pediatrics at the University of Maryland School of Medicine for eight years prior to returning to Children’s National. Her research interests have focused on using near-infrared spectroscopy to evaluate hemodynamic status and cerebral autoregulation in premature infants in relationship to outcomes. More recently, she is partnering with the Advanced Signals Processing Lab to evaluate autonomic development in premature infants in relationship to respiratory outcomes. In addition, she oversees the education and simulation curriculum and is currently pursuing an advanced degree in medical education.
Panagiotis Kratimenos, MD
Associated Facility: Children's National Hospital
Dr. Kratimenos is a neonatologist and developmental neuroscientist whose research focuses on elucidating mechanisms of perinatal brain injury. Dr. Kratimenos studies mechanisms of injury of the developing cerebellum with the goal of developing therapeutic interventions and improving functional development.
Lauren Miyares, MD
Associated Facility: George Washington Hospital
Dr. Miyares earned her medical degree from The George Washington University School of Medicine and Health Sciences. She then went on to complete both her pediatric residency and Neonatal-Perinatal fellowship at Children’s National Hospital. Her academic interests are rooted in medical education, and she currently serves as the associate program director for the GW portion of the Neonatal-Perinatal Fellowship Program.
Hallie Morris, MD
Associated Facility: Children's National Hospital & George Washington Hospital
Hallie Morris, MD, joined the Children's National team from the Washington University in St. Louis program where she was involved in their neonatal brain research program, with plans to participate in the Children’s National clinical Neo-Neuro Program. She also has expertise in Quality/Safety methodologies and will be joining the strong QI/Safety program in the NICU. She is also one of our attendings rotating between our Perinatal Center at George Washington University Hospital NICU and CN Level IV NICU, with expertise in perinatal medicine.
Nneka Nzegwu, DO, MPH
Associated Facility: Children's National Hospital
Dr. Nzegwu is the associate director of quality and safety for the Division of Neonatology. Her area of interest is using quality improvement methodologies to improve the care of our patients at the bedside. Her areas of focus are preventing hospital-acquired conditions, neonatal nutrition and antibiotic stewardship in the NICU. She enjoys educating and mentoring residents, fellows and colleagues about quality improvement science and patient safety principles.
Katherine Marie Ottolini, MD
Associated Facility: Children's National Hospital & George Washington Hospital
Dr. Ottolini is a neonatologist at Children’s National Hospital and assistant professor of pediatrics at The George Washington University School of Medicine and Health Sciences. She completed pediatric residency at Walter Reed National Military Medical Center and Neonatal-Perinatal fellowship at Children’s National Hospital. Following completion of fellowship training, she served as a neonatologist in the U.S. Air Force in Okinawa, Japan, for four years prior to returning to Children’s National. Her research through the Developing Brain Institute is aimed at optimizing neurodevelopmental outcomes in preterm infants through early nutritional interventions.
Khodayar Rais-Bahrami, MD
Associated Facility: Children's National Hospital
Dr. Rais-Bahrami is the director of the Neonatal-Perinatal Fellowship Program and professor of pediatrics at The George Washington University School of Medicine and Health Sciences. His major focus is to ensure that fellows are matched with mentors who will assure their success in clinical and/or bench research, while directing their long-term goals for their fellowship training. His clinical and research interest include research into the evaluation of devices being considered for use in the neonatal population, including the NIRS system for brain and enteric monitoring of oxygenation in the neonatal population. Other interests include evaluation of wireless cardiovascular monitoring systems to be used both in the NICU and as home monitors, and recent investigation of a novel non-invasive cardiovascular monitor systems used to measure cardiac output, blood volume and ductal shunt in the neonatal population as well as cardiac output and recirculation measurements in neonatal ECMO population. He has mentored numerous fellows in projects in these areas and as director of the Neonatal-Perinatal Fellowship Program, he continues to be committed to mentoring the research development of young fellows and investigators at different levels of training who work synergistically to answer critical questions in neonatology.
Mary Revenis, MD
Associated Facility: Children's National Hospital
Dr. Revenis is an neonatologist at Children’s National Hospital and a clinical professor at The George Washington University School of Medicine and Health Sciences. She completed pediatric residency at Montefiore Medical Center and completed neonatal-perinatal fellowship at Children’s National Hospital. She is active in the D.C. AAP, is Chair of the DC AAP Fetus and Newborn Committee and is a member of several DC DOH committees. She is passionate about infant mortality reduction, organ/tissue donation, newborn nutrition and breastfeeding, immunizations, newborn screening, NICU sustainability and early childhood literacy and education. She is the medical director of Nutrition Services in the NICU. She also collaborates with the Division of Nephrology in multicenter studies on acute renal failure in the newborn and is an advocate for access to renal therapy and follow-up.
Billie Lou Short, MD
Associated Facility: Children's National Hospital
Dr. Short is chief of the Division of Neonatology is responsible for overseeing the division’s clinical and research efforts. Her background has been in the area of brain physiological changes related to therapies such as extracorporeal membrane oxygenation (ECMO), and clinical studies in analyzing outcome related to brain injury in this population. She provides leadership on the international Children’s Hospitals Neonatal Consortium Executive Board, which organizes and initiates multicenter quality outcome research programs across the nation.
Lamia Soghier, MD, FAAP, CHSE
Associated Facility: Children's National Hospital
Dr. Soghier is the associate chief of Neonatology for operations and the medical director and NICU quality and safety officer. She is a professor of pediatrics at The George Washington University School of Medicine and Health Sciences. Her areas of interest are medical education, specifically improvement of procedural skills through simulation and technology, and the use of simulation for quality improvement. She has sponsored and published several quality improvement initiatives. Currently, Dr. Soghier focuses on improving parental mental health and has mentored and supervised projects led by residents and fellows. Her current funding includes grants from AHRQ, Clark Family Foundation, Center for Translational Research and others to study improvement in postpartum mood and anxiety screening in the NICU and pediatric Emergency Department.
Simranjeet Sran, MD
Associated Facility: Children's National Hospital
Dr. Sran's interests are focused on medical education for trainees and medical students. He recently graduated with a master’s degree in education and human development from George Washington University, creating a curriculum for daily education of pediatric residents rotating through the NICU. For our fellows, Dr. Sran helps develop curricula and facilitate weekly Fellow Education Sessions through his role as director of education for the division. He is the rotation director for pediatric residents, director of education for the hospital-wide Simulation Program, and co-director of the Practice of Medicine course at The George Washington University School of Medicine and Health Sciences.
Lakshmi Sridhar, MD
Associated Facility: Children's National Hospital
Dr. Sridhar joined the Children’s National team after completing her Neonatal-Perinatal Medicine fellowship along with a M.S. in health professions education at the University of Rochester. Prior, she completed pediatric internship, residency and chief residency at Children's Hospital of New Jersey (Rutgers-RWJ-Newark Beth Israel). Her clinical and research interests are in telesimulation, distance learning, simulation, education, point-of-care ultrasound and quality improvement. She is a part of our nocturnal neonatal attending team.
Keisha Dale Wolfe, DO
Associated Facility: George Washington Hospital
Dr. Wolfe joined the Children’s National team after completing her fellowship in Neonatal-Perinatal Medicine at Georgetown University Hospital. She completed her pediatrics residency at Naval Medical Center at Portsmouth, VA, and served as general pediatrician for the U.S. Air Force prior to her fellowship. Her research background included neonatal studies in probiotics and the immune system, the gut microbiome, and hyperbilirubinemia as well quality improvement. Her ongoing research interests include nutrition, growth, POCUS and QI. She enjoys teaching residents, fellows and NICU staff and has been a long standing instructor for NRP and STABLE. She is a part of our nocturnal neonatal attending team and rotates at the George Washington University NICU.




