Bringing Trusted Pediatric Colorectal Care to Children Worldwide
Our program offers virtual consultations, allowing us to provide expert care to patients anywhere in the world. No matter where you are, we are committed to delivering personalized medical support right to your location.

Our Providers
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs.
Why Choose Us for Pediatric Colorectal and Pelvic Reconstruction?
As the only pediatric colorectal and pelvic reconstructive program in the nation with this level of expertise, there are many reasons to choose Children’s National for your child’s treatment and care. In addition to our integrated team, we offer:
- Access to the most experienced and renowned pediatric colorectal specialists in the field.
- Exceptional surgical expertise for even the most complex colorectal disorders.
- Dedicated, compassionate nurses, nurse practitioners and physician associates who are specially-trained in caring for patients with complex pediatric colorectal disorders.
- The latest advanced diagnostic and surgical treatment, using minimally invasive techniques.
- A comprehensive Bowel Management Program to help achieve optimal bowel function.
- Colorectal care for life through the Colorectal Transition Program

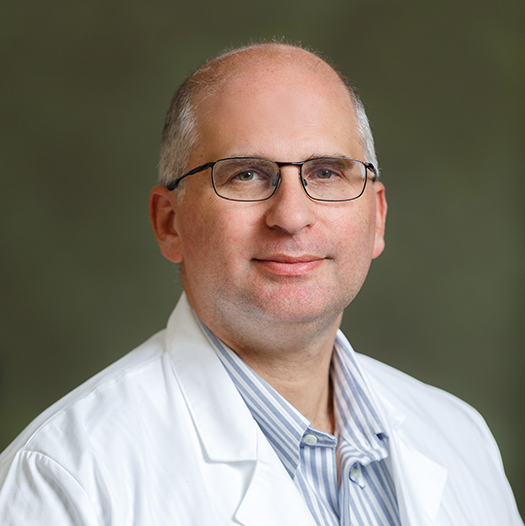
Dr. Levitt's Expertise in Cloacal Malformation
Over the past 25 years, Marc Levitt, MD, has performed over 1,000 cloacal reconstructions for patients with a cloacal malformation, the operation for which is called a Posterior Sagittal Anorectal Vagino-Urethroplasty (PSARVUP). This is the most technically difficult pediatric colorectal operation and requires unique experience and expertise. This number exceeds any other pediatric colorectal surgeon in the world. Dr. Levitt has also authored the textbook on the subject (shown above).

Colorectal Procedures By the Numbers
Marc Levitt, MD, and the Division of Colorectal & Pelvic Reconstruction at Children’s National Hospital are leading the world in caring for pediatric patients with colon, rectal and pelvic conditions. In addition to the procedures listed here, the team also has vast experience in “redo” operations or surgeries. These “redo” surgeries are needed when a patient’s previous surgery took place at another hospital, and now the anatomy needs corrections to improve the possibility of bowel control.
Dr. Levitt and his teams have performed over:

2,000+
Posterior Sagittal Anorectoplasties (PSARPs) during the past 25 years (including 400+ since joining Children's National in 2019) | This procedure is a repair for children with imperforate anus/anorectal malformations (ARM).
1,000+
Pull-Through Surgeries during the past 25 years (including 200+ since joining Children's National in 2019) | This procedure is for patients with Hirschsprung's disease. We handle one to two such cases per week.
500+
Malone Appendicostomies during the past 25 years (including 50+ annually since joining Children's National in 2019) | This operation helps children with fecal incontinence, ultimately helping some achieve their own bowel control.
Our Unique Approach to Pediatric Colorectal Disorders
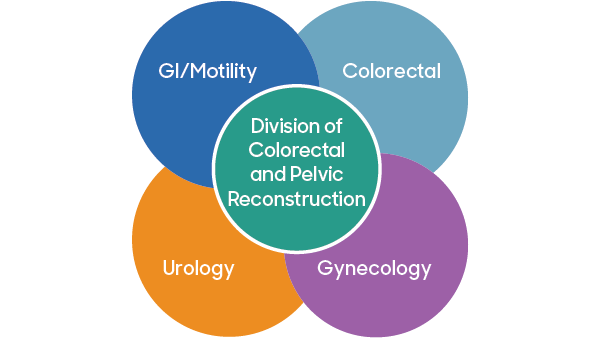
Integrated Care
Our multidisciplinary Division of Pediatric Colorectal & Pelvic Reconstruction integrates services across all the specialties that provide care for colorectal conditions in children. Colorectal procedures are often combined with urologic and gynecologic procedures to minimize the amount of surgeries a child may require.
Our division is led by world-renowned pediatric colorectal surgeon, Marc Levitt, MD, who has expertise in treating the full spectrum of pediatric colorectal conditions and has performed over 15,000 surgeries — more than any other surgeon trained in pediatric colorectal surgery worldwide. Learn more about Dr. Levitt and our Division of Colorectal & Pelvic Reconstruction.
Our collaborative approach offers treatment from experts across multiple medical disciplines, including:

Getting Ready for Your First Appointment?
To streamline the process, we strongly encourage that you complete our intake form. Once your child’s medical records have been received, we will review their information and contact you to schedule an appointment.

Ask Dr. Levitt About Your Child's Diagnosis
Was your newborn child recently diagnosed with an anorectal malformation, imperforate anus, cloaca or Hirschsprung's disease? If so, Marc Levitt, MD, is here to provide answers to your questions.

Our Specialized Programs

Bowel Management Program
We offer a comprehensive Bowel Management Program that provides customized treatment for children who experience fecal incontinence.

Colorectal Transition Program
The Colorectal Transition Program helps children with congenital or acquired colorectal conditions transition their care from pediatric care providers to adult care providers.

Pelvic Physical Therapy Program
Our Pelvic Physical Therapy (PT) Program provides children and adolescents with pelvic floor dysfunction the guidance and coaching they need to optimize functioning of the pelvic floor muscles.

Conditions We Treat
Understanding your child's condition is an important step on your treatment journey. Learn more about the causes, symptoms and diagnosis for a variety of pediatric colorectal conditions, as well as unique treatments and research being performed at Children's National Hospital.
Treatments & Resources
Review these materials to find out more about the diagnosis, treatment and other aspects of your child's condition.

Caring for Your Child's Colorectal Disorder
Learn how to care for your child from diagnosis to treatment, all the way through long-term aftercare.

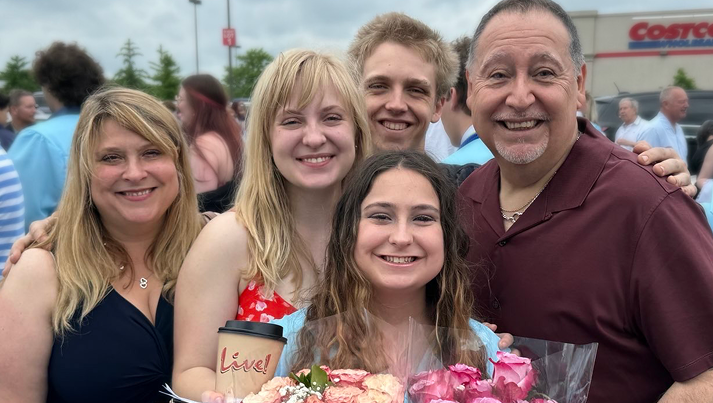
Colorectal Employee Stories
Learn about the stories and experiences of team members in the colorectal program.