Bella's Story

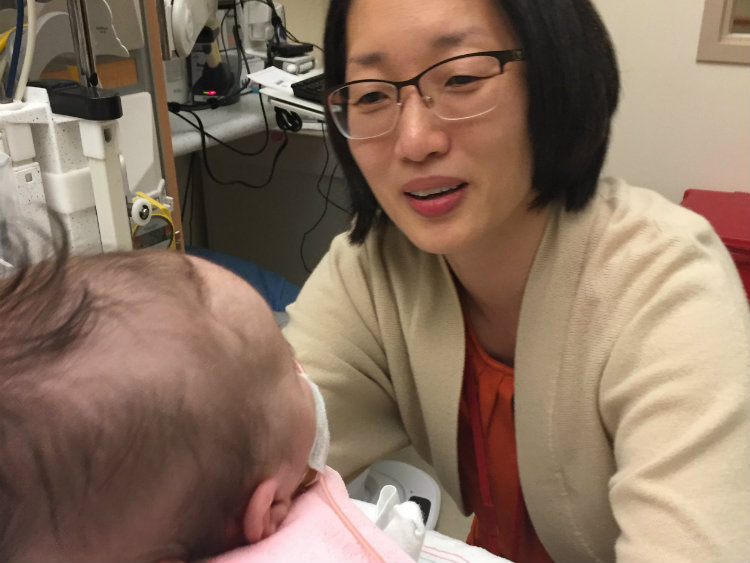
Have courage. That’s what Taeun Chang, M.D., counseled David and Ann Getting as they debated a fateful decision about their first grandchild’s future. Bella Grace was born Thursday, Aug. 16, 2018, in Ames, Iowa. On that first day, she seemed normal. Everything seemed perfect.
The second day, slight twitching was observed in Bella’s eyes. Testing revealed that Bella’s brain was abnormal on the left side. The family was informed that Bella would be transferred to Des Moines immediately. The Gettings’ family friend, pediatrician Dr. Amy Mashburn (who they call “Dr. Amy”) dropped everything to fly from Kentucky to be by the couple’s side.
The Des Moines hospital lacked the right person to read the brain magnetic resonance image (MRI). Bella was transferred to a third hospital one mile away on Saturday. That’s when the Gettings learned Bella had hemimegalencephaly (HME), a rare brain disorder in which one half of the brain grows abnormal and large and misbehaves by triggering repeated difficult seizures.
“Bella was only a couple of days old. It was devastating news. They told us about all kinds of potential disabilities. They also said it would be extremely difficult to control her seizures with medications,” recalls Ann Getting. “They didn’t have this kind of patient come along very often. Only one doctor in their neonatal intensive care unit (NICU) had seen another case of HME.”
The medical team explained the traditional textbook approach – waiting a few months until Bella was big enough and strong enough to survive dramatic surgery to remove half of her brain.
“The standard practice is cut her open and do a full hemispherectomy when she was at least 3 months old,” says David Getting. “Her seizures were so bad, her quality of life would have been negatively impacted if we waited.”
By that point, Bella’s electroencephalogram (EEG) indicated that she was experiencing 20 to 40 seizures per hour, non-stop, despite several seizure medications. Every month delay meant a 10- to 20-point drop in Bella’s IQ.
When her family learned the standard treatment meant waiting three months for surgery, they wanted a better option for Bella. Then the Gettings learned about an innovative approach at Children’s National Hospital. Bella’s family decided giving Bella this opportunity was worth the 1,000-mile trip to Washington, D.C., they said, because they had hope that the team at Children’s National could give Bella a chance to be all she could be.
Go, Bella, go!
Bella is doing well, amazing her family in Iowa and delighting her Children’s National Hospital care team in Washington, D.C. Bella has not experienced a seizure in more than one year, thanks to an innovative, non-surgical procedure pioneered by Children’s National.